An analysis of grievances filed by beneficiaries of Ayushman Bharat has shown that the highest number were about hospitals demanding money for treatment. This entailed unexpected out-of-pocket expenditure (OOPE) though the scheme was meant to provide cashless hospitalisation and bring down out of pocket expenses.
A 2023 CAG report too had noted that 75 out of the 121 healthcare providers de-empanelled from 2018 to 2021 were found to be engaged in illegal money collection and other fraudulent practices.
According to a paper published by Centre for Health Equity, Law and Policy and the Association for Socially Applicable Research, Chhattisgarh, Jharkhand and Uttarakhand topped the list for grievances related to the quality of hospital services, and Maharashtra, Assam and Bihar led in eligibility and registration issues. Uttar Pradesh, Bihar and Madhya Pradesh had the highest proportion of grievances related to poor behaviour of hospital and programme staff and related to quality of programmatic service.
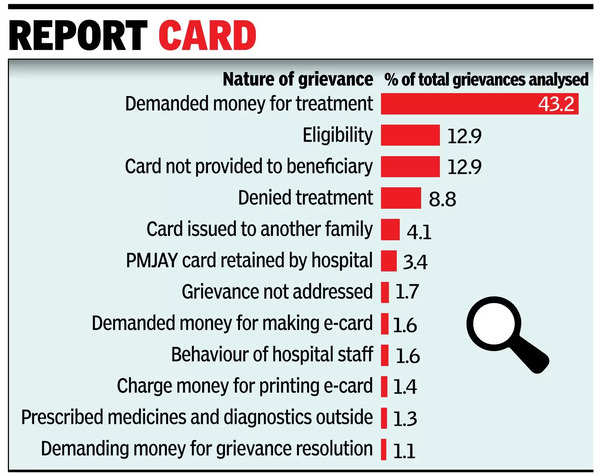
“While the majority of grievances about hospital service quality were due to hospitals demanding money for treatment, most grievances related to eligibility and registration stemmed from problems with the issuance of beneficiary cards,” stated the study.
The paper published in the Social Science Research Network of Elsevier, an open-access online preprint community and repository, examined a total of 1.1 lakh grievances filed by beneficiaries under the AB-PMJAY grievance redress system from Oct 2018 to March 2022 at the national, state and district levels. However, 67% of the grievances were categorised as ‘other’ and could not be included in the analysis. This was also true of those categorised as ‘inquiry’ or ‘feedback’, which were another 3%. “We filed an RTI with the National Health Authority to find out what ‘other’ meant, but were told that this was the category chosen by the beneficiary,” explained Shefali Malhotra, one of the authors of the paper.
Though quality of hospital services constituted the highest proportion of grievances analysed, those related to registration and eligibility for the Ayushman card constituted the highest proportion during the Covid years. Within complaints about quality of hospital services, 74% was related to the hospital demanding money. Other reasons included denial of treatment (15%), hospitals holding onto ABPMJAY cards 6%, non-availability of medicines and diagnostics in the hospital (2.2%), and poor quality of treatment (2%).
“The incidence of grievances in Assam was markedly higher than in other states and union territories participating in the AB-PMJAY programme, throughout the study period. About 52% of these grievances were associated with eligibility and registration issues under the scheme. Possible reasons for this are highlighted in the 2023 CAG report, which points out considerable delays, 187 days on average, in the approval and rejection of beneficiaries’ registration,” noted the study adding that this could be attributed to the 70% manpower shortage in the state health agency as flagged by the CAG.
